How To Fix Seborrheic Dermatitis On The Face

Seborrheic dermatitis is a chronic inflammatory disorder affecting areas of the head and torso where sebaceous glands are most prominent. Lipophilic yeasts of the Malassezia genus, as well every bit genetic, ecology and full general wellness factors, contribute to this disorder. Scalp seborrhea varies from balmy dandruff to dumbo, diffuse, adherent calibration. Facial and trunk seborrhea is characterized by powdery or greasy calibration in peel folds and along pilus margins. Treatment options include application of selenium sulfide, pyrithione zinc or ketoconazole-containing shampoos, topical ketoconazole cream or terbinafine solution, topical sodium sulfacetamide and topical corticosteroids.
The etiology of seborrheic dermatitis remains unknown, although many factors, including hormonal, have been implicated. This chronic inflammatory skin disorder is generally bars to areas of the caput and torso where sebaceous glands are most prominent. When seborrheic dermatitis occurs in the neonatal period, it usually disappears by half-dozen to 12 months of historic period, suggesting that information technology may be a response to maternal hormone stimulation.1
Seborrheic dermatitis frequently affects persons in postpuberty. Additional evidence of hormonal influence is provided past research demonstrating that the homo sebocyte responds to androgen stimulation.2
Pityrosporum ovale, a lipophilic yeast of the Malassezia genus, has been implicated in the development of this condition.3 It has been suggested that seborrheic dermatitis is an inflammatory response to this organism, but this remains to exist proved.iv P. ovale is present on all persons. Why some persons develop seborrheic dermatitis and others practice non is unclear. The colonization rate of involved skin by this organism may be lower than that of uninvolved pare.3 Nonetheless, the fact that seborrheic dermatitis responds to antifungal medications is strongly suggestive of the role of yeast in this disorder.
Genetic and environmental factors, as well equally other comorbid diseases, may predispose specific populations to the development of seborrheic dermatitis. Although seborrheic dermatitis affects only 3 percent of the general population, the incidence in persons with acquired immunodeficiency syndrome may be as high as 85 per centum. The exact mechanism whereby human immunodeficiency virus infection promotes an atypical and explosive onset of seborrheic dermatitis (and other common inflammatory pare disorders) is unknown, merely many factors have been explored, including CD4-positive T lymphocyte counts,5 P. ovale density6 and nutritional factors.7
Persons with central nervous system disorders (Parkinson's disease, cranial nerve palsies, major truncal paralyses) also appear to be decumbent to the development of seborrheic dermatitis, tend to develop more than extensive disease and are oft refractory to treatment. Information technology has been postulated that seborrheic dermatitis in these patients is a result of increased pooling of sebum caused by immobility. This increased sebum pool permits growth of P. ovale, which induces seborrheic dermatitis.viii
Clinical Manifestations
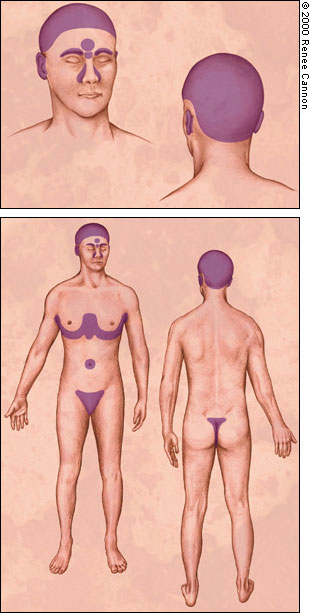
Seborrheic dermatitis typically affects areas of the skin where sebaceous glands appear in high frequency and are most agile. The distribution is classically symmetric, and common sites of involvement are the hairy areas of the head, including the scalp (Figure 1), the scalp margin (Effigy two), eyebrows, eyelashes, mustache and beard. Other common sites are the brow (Figure 3), the nasolabial folds (Effigy iv), the external ear canals (Figure v) and the postauricular creases. Seborrhea of the trunk may announced in the presternal surface area (Effigy 6) and in the torso folds, including the axillae, umbilicus, groin, and in the inframammary and anogenital areas. Effigy 7 illustrates the typically symmetric distribution of seborrheic dermatitis.






I of the characteristics of seborrheic dermatitis is dandruff, characterized by a fine, powdery white scale on the scalp. Many patients complain of the scalp itching with dandruff, and because they recollect that the scale arises from dry peel, they decrease the frequency of shampooing, which allows further scale accumulation. Inflammation and so occurs and their symptoms worsen.
More astringent seborrheic dermatitis is characterized by erythematous plaques oft associated with powdery or greasy calibration in the scalp (Effigy 8), behind the ears (Effigy nine) and elsewhere in the distribution described above. Likewise an itchy scalp, patients may complain of a burning sensation in facial areas affected by seborrhea. Seborrhea frequently becomes apparent when men grow mustaches or beards and disappears when the facial hair is removed. If left untreated, the scale may get thick, yellow and greasy and, occasionally, secondary bacterial infection may occur.


Seborrheic dermatitis is more common in men than in women, probably considering sebaceous gland activeness is under androgen control. Seborrhea commonly first appears in persons in their teens and twenties and more often than not follows a waxing/waning class throughout machismo.
UV-A and UV-B calorie-free inhibit the growth of P. ovale,9 and many patients report improvement in seborrhea during summer.
Treatment
GENERAL Treatment OVERVIEW
Hygiene problems play a fundamental role in decision-making seborrheic dermatitis. Frequent cleansing with soap removes oils from affected areas and improves seborrhea. Patients should be counseled that good hygiene must exist a lifelong commitment. Outdoor recreation, specially during summertime, volition likewise improve seborrhea, although caution should be taken to avoid sun damage.
Pharmacologic handling options for seborrheic dermatitis include antifungal preparations (selenium sulfide, pyrithione zinc, azole agents, sodium sulfacetamide and topical terbinafine) that decrease colonization by lipophilic yeast and anti-inflammatory agents (topical steroids). Suggested products are listed in Table 1. For astringent affliction, keratolytics such as salicylic acid or coal tar preparations may exist used to remove dense scale; and so topical steroids may be applied. Other options for removing adherent calibration involve applying whatever of a variety of oils (peanut, olive or mineral) to soften the calibration overnight, followed by use of a detergent or coal tar shampoo.
Every bit a last resort in refractory disease, sebosuppressive agents such as isotretinoin (Accutane) may be used to reduce sebaceous gland activity.
Handling OF SCALP AND Beard AREAS
Many cases of seborrheic dermatitis are effectively treated by shampooing daily or every other day with antidandruff shampoos containing 2.five percent selenium sulfide or one to ii pct pyrithione zinc. Alternatively, ketoconazole shampoo may be used.10 The shampoo should be practical to the scalp and beard areas and left in place for five to 10 minutes before rinsing. A moisturizing shampoo may be used after to forestall dessication of the pilus. After the illness is under control, the frequency of shampooing with medicated shampoos may exist decreased to twice weekly or as needed. Topical terbinafine solution, 1 percent, has also been shown to exist constructive in the handling of scalp seborrhea.11
If the scalp is covered with lengthened, dense scale, the scale may get-go exist removed by applying warm mineral oil or olive oil to the scalp and washing several hours later with a detergent such as a dishwashing liquid or a tar shampoo.12 An alternative is an overnight awarding of a coal tarkeratolytic combination or phenol-saline solution with or without apoplexy with a plastic shower cap followed by shampooing in the forenoon.13
All-encompassing scale with associated inflammation may be treated past moistening the scalp and so applying fluocinolone acetonide, 0.01 percentage in oil, to the unabridged scalp, covering overnight with a shower cap and shampooing in the morning. This handling may be done nightly until the inflammation clears so decreased to one to three times weekly as needed. Topical corticosteroid solutions, lotions or ointments may be used once or twice daily for 1 to iii weeks in place of the overnight awarding of fluocinolone acetonide and may be stopped when itching and erythema disappear. Corticosteroid application may be repeated daily for one to 3 weeks until itching and erythema disappear, and then used as needed. Maintenance with an antidandruff shampoo may then exist acceptable. Patients should exist advised to employ potent topical steroids sparingly because excessive employ may pb to atrophy of the pare and telangiectasis.
Infants oft have seborrheic dermatitis, unremarkably known as "cradle cap." Areas of possible involvement include the scalp, face and intertriginous areas. Interest may be extensive, but this disorder frequently clears spontaneously by vi to 12 months of age and does not recur until the onset of puberty.
A scaly scalp in a prepubertal child is unremarkably caused by tinea capitis, non seborrheic dermatitis. Therapy for infantile seborrheic dermatitis includes frequent shampooing with an antidandruff shampoo. If scale is extensive in the scalp, the scale may exist softened with oil, gently brushed free with a baby hairbrush and then done articulate.
Daily shampooing may non be reasonable for some populations, such as black persons or persons who are institutionalized. In general, weekly shampooing is recommended for black persons. As a substitute for daily washing, fluocinolone acetonide, 0.01 percent in oil, may exist used as a scalp pomade. Other options include application of a moderate- to mid-potency topical corticosteroid in an ointment base of operations. As with other modes of therapy, these agents are used every day or twice daily until the status improves. Thereafter, topical corticosteroids are used equally needed to go on the status under command. After initial control is attained, fluocinolone acetonide, 0.01 percent shampoo (FS Shampoo), can be used as an alternative to or in addition to fluocinolone acetonide, 0.01 percentage in oil (Derma-Smoothe/FS), for maintenance.
Treatment OF THE FACE
Involved areas of the face may be washed frequently with shampoos that are effective against seborrhea every bit detailed above. Alternatively, ketoconazole foam, 2 percent, may be practical one time or twice daily to affected areas. Often, 1 per centum hydrocortisone cream will be added one time or twice daily to afflicted areas and will help with resolution of erythema and itching. Sodium sulfacetamide, x percentage balm, is also an effective topical agent for seborrheic dermatitis.
TREATMENT OF THE Torso
Seborrhea of the trunk may be treated with frequent awarding of zinc or coal tar containing shampoos or by washing with zinc soaps. Additionally, topical ketoconazole foam, 2 percent, and/or a topical corticosteroid cream, lotion or solution practical once or twice daily volition bear witness useful. Benzoyl peroxide washes are also helpful in controlling seborrhea of the body. Patients should be cautioned to rinse thoroughly after awarding of these agents as they will bleach vesture and bed linens. These agents may be drying, and the patient may benefit from awarding of a moisturizer later on treatment.
TREATMENT OF SEVERE SEBORRHEA
An occasional patient with severe seborrhea that is unresponsive to the usual topical therapy may be a candidate for isotretinoin therapy.xiv Isotretinoin tin induce up to a 90 percent reduction in sebaceous gland size, with a corresponding reduction in the production of sebum. Isotretinoin also has anti-inflammatory properties. Treatment with daily doses of isotretinoin as low every bit 0.1 to 0.3 mg per kg may consequence in improvement in astringent seborrhea after four weeks of therapy. Thereafter, a dose every bit low as 5 to 10 mg per twenty-four hours may exist effective as maintenance therapy over several years. Even so, isotretinoin has potentially serious side effects and few patients with seborrhea are appropriate candidates for therapy. The most devastating side effect is teratogenicity, but other serious side furnishings include hyperlipidemia, neutropenia, anemia and hepatitis. Mucocutaneous adverse furnishings include cheilitis, xerosis, conjunctivitis, urethritis and hair loss. Long-term use has been associated with the evolution of diffuse idiopathic skeletal hyperostosis (DISH). This agent must be used cautiously and only by physicians who are well versed in all of its adverse effects.
A more practical approach to the refractory patient may be to first effort different combinations of the usual agents: a dandruff shampoo, an antifungal agent and a topical steroid. If this fails, curt-term use of a more potent topical steroid in a "pulse mode" may put some refractory patients into remission and actually decrease the total steroid exposure. Therapeutic choices for pulse therapy may include a nonfluorinated course III steroid such as mometasone furoate (Elocon) or an extra-potent class I or class Ii topical steroid such as clobetasol propionate (Temovate) or fluocinonide (Lidex). The class III topical steroid should be tried first, just if the condition remains unresponsive, the clinician may then choose to use a class I amanuensis. These more potent agents may be applied once or twice per day, fifty-fifty on the face, but must be stopped subsequently two weeks because of the increased frequency of side furnishings. If the patient responds earlier the two-week limit, the agent should be stopped immediately. Adjuvant therapy including use of a dandruff shampoo, an anti-fungal agent, or both, is essential during the "pulse" period and should be connected as maintenance therapy after each pulse.
Most corticosteroids are available as solutions, lotions, creams and ointments. Which vehicle to use is frequently determined past the patient and the treatment site. Lotions and creams are frequently used on all areas of the face and body, whereas solutions and ointments are more commonly used on the scalp. In general, awarding of a scalp solution is preferred by white and Asian patients merely may be also drying for black patients. Ointments may be a better option. The vehicle affects the authority of a topical steroid. In most circumstances, the same steroid in an ointment is more potent than the steroid in a cream, which, in plow, is more strong than the same chemic in a lotion.
When to Refer
Patients should be referred to a dermatologist if the diagnosis is in dubiety or if they are not responding to treatment. Seborrhea may exist hard to distinguish from atopic dermatitis, psoriasis, rosacea or superficial fungal infections. Chronic handling with topical corticosteroids may pb to permanent skin changes, such equally atrophy and telangiectasia. The explosive onset of seborrheic dermatitis in a young patient should give rise to consideration of underlying man immunodeficiency virus infection. 1 should consider referral to a dermatologist for patients with severe seborrhea in whom handling with oral isotretinoin is contemplated, particularly if long-term therapy will probable be required.
How To Fix Seborrheic Dermatitis On The Face,
Source: https://www.aafp.org/pubs/afp/issues/2000/0501/p2703.html
Posted by: sanchezyournegand.blogspot.com


0 Response to "How To Fix Seborrheic Dermatitis On The Face"
Post a Comment